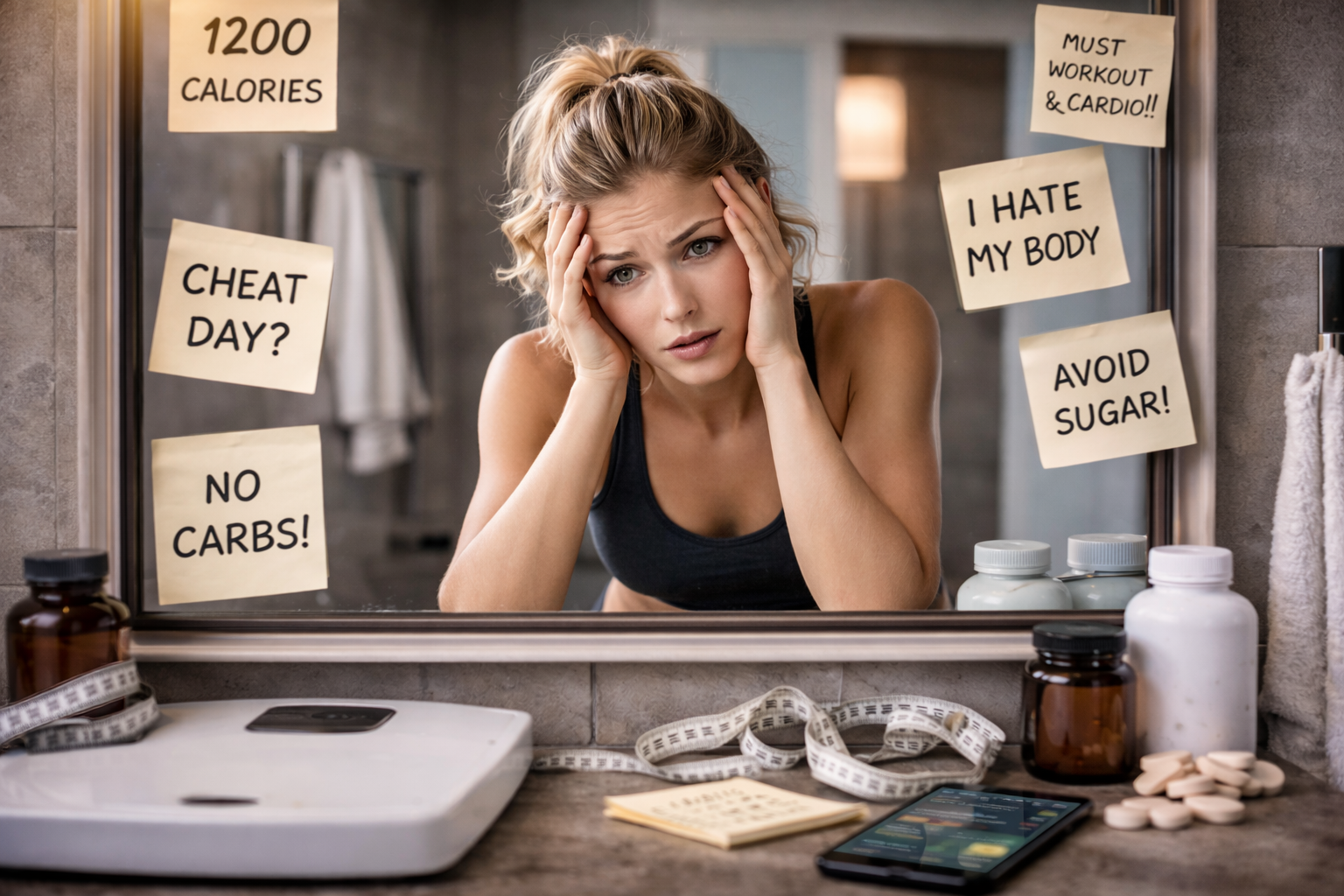
In fitness-driven environments, discipline is praised, leanness is normalized, and constant dietary control is often framed as commitment. But beneath the surface, chronic dieting carries a psychological cost that many active adults overlook—one that can quietly erode mental health, performance, and long-term well-being.
While short-term energy restriction can serve a purpose, repeated or prolonged dieting cycles are strongly associated with increased psychological stress, disordered eating behaviors, mood disturbances, and reduced quality of life.
This article examines what chronic dieting really does to the brain, why fitness-focused adults are particularly vulnerable, and how to pursue body composition goals without sacrificing mental health.
What Is Chronic Dieting?
Chronic dieting refers to repeated or ongoing attempts to restrict energy intake, often driven by physique goals rather than medical necessity. In fitness-focused populations, this may include:
- Frequent cutting phases
- Long-term calorie suppression
- Rigid food rules or macro fixation
- Persistent fear of weight gain
- Cycles of restriction followed by loss of control
Unlike structured performance nutrition phases, chronic dieting often lacks recovery periods, psychological flexibility, and metabolic recalibration.
The Cognitive Burden of Constant Food Control
1. Mental Preoccupation With Food and Body Image
Caloric restriction increases food-related thoughts, attentional bias toward eating cues, and body surveillance, even in physically active individuals. Over time, this cognitive load can reduce focus, motivation, and enjoyment of training.
Research shows that restrained eaters exhibit:
- Increased rumination about food
- Heightened guilt after eating
- Reduced interoceptive awareness
These patterns persist even when body weight is stable.
Mood Disturbances and Emotional Dysregulation
Chronic dieting is associated with:
- Increased irritability and anxiety
- Depressive symptoms
- Emotional blunting during prolonged restriction
Disordered Eating Risk in Fitness-Focused Adults
While not synonymous with eating disorders, chronic dieting significantly increases risk for:
- Binge-restrict cycles
- Orthorexic tendencies
- Compulsive tracking behaviors
Athletes and fitness professionals show higher rates of subclinical disordered eating than the general population, largely due to normalization within training culture.
➡️ Why Motivation Is a Poor Strategy for Long-Term Fitness Success
Weight Cycling and Psychological Fatigue
Repeated dieting attempts often lead to weight cycling, which is independently associated with:
- Reduced self-efficacy
- Increased body dissatisfaction
- Heightened stress response
Weight cycling also reinforces the belief that stricter control is required for success—further entrenching dieting behaviors.
➡️ Why Recovery Is the Missing Variable in Most Fat-Loss Programs
Identity Conflict in Fitness Culture
For many fitness-focused adults, body composition becomes tied to personal identity, credibility, and self-worth. Chronic dieting reinforces a narrow definition of success, making flexibility feel like failure.
This identity-performance conflict often results in:
- Training through fatigue
- Ignoring hunger and recovery cues
- Anxiety during unstructured eating periods
➡️ The Weight Loss and Wellness Connection
The Physiological–Psychological Feedback Loop
Chronic energy restriction creates a self-reinforcing loop:
- Reduced energy availability
- Hormonal disruption (leptin, thyroid, cortisol)
- Increased psychological stress
- Reduced training quality and recovery
- Heightened control behaviors
Breaking this cycle requires periodized nutrition, not perpetual restraint.
Sustainable Alternatives to Chronic Dieting
Evidence-based strategies include:
- Diet periodization with defined recovery phases
- Performance-anchored nutrition targets
- Outcome-neutral habit tracking
- Emphasis on training quality, not constant leanness
- Psychological flexibility around food
➡️ Electrolytes, Sodium, and Performance: How Much Is Actually Needed?
These approaches shift focus from control to capacity, recovery, and longevity.
Key Takeaways
- Chronic dieting imposes real psychological costs, even in fit individuals
- Mental health, recovery, and performance are tightly interconnected
- Fitness culture often normalizes unsustainable behaviors
- Long-term success requires nutritional flexibility and psychological safety
True fitness is not defined by perpetual restriction—but by resilience, adaptability, and sustainability.
References
Dulloo, A. G., Jacquet, J., Montani, J. P., & Schutz, Y. (2015). Adaptive thermogenesis in human body weight regulation: More of a concept than a measurable entity? Obesity Reviews, 16(S1), 5–17.
Herman, C. P., & Polivy, J. (2011). The self-regulation of eating: Theoretical and practical problems. Journal of Social and Clinical Psychology, 30(2), 117–137.
Loucks, A. B., Kiens, B., & Wright, H. H. (2011). Energy availability in athletes. Journal of Sports Sciences, 29(S1), S7–S15.
Mann, T., Tomiyama, A. J., Westling, E., Lew, A. M., Samuels, B., & Chatman, J. (2007). Medicare’s search for effective obesity treatments: Diets are not the answer. American Psychologist, 62(3), 220–233.
Polivy, J., & Herman, C. P. (2020). Restrained eating and food cues: Recent findings and conclusions. Current Obesity Reports, 9(1), 79–85.
Sundgot-Borgen, J., & Torstveit, M. K. (2010). Aspects of disordered eating continuum in elite high-intensity sports. Scandinavian Journal of Medicine & Science in Sports, 20(S2), 112–121.